The Pulse
COVID-19: Protection for Health Care Workers During the New Wave
Category: COVID-19, Healthcare Industry
IN A NUTSHELL:
- Know how to wear and remove personal protective equipment
- Transmission shown to occur via respiratory droplets among close contacts
- EMS drivers should take extra precautions to isolate themselves during transport
- CME Course: Identification and Containment of the Coronavirus: COVID-19
After more than nine months, researchers are still learning about the novel Coronavirus, the virus that causes COVID-19, including how easily it spreads.
However hope is now on the horizon, as Pfizer and Moderna have announced promising interim results for their vaccine candidates, the latter of which may be 95% effective.
While neither of the vaccines have been authorized for use by the U.S. FDA, if and when they do distribution will be a major challenge due to their storage requirements. The vaccine made by Pfizer needs to be kept extremely cold—at a temperature of minus 70 degrees Celsius. The vaccine produced by Moderna needs to be frozen too, but only at minus 20 Celsius, more like a regular freezer.
What is known about the Coronavirus:
The novel coronavirus can easily spread from person to person. Symptoms of COVID-19 can range from asymptomatic, mild, to severe illness and even death.
How it can spread:
You can become infected by coming into close contact (about 6 feet or two arm lengths) with a person who has COVID-19. COVID-19 is primarily spread from person to person by respiratory droplets when an infected person coughs, sneezes, or talks. It is also possible to become infected by touching a surface or object that has the virus on it, and then by touching your mouth, nose, or eyes.
Impact on health care workers:
Health care workers are on the front lines of caring for patients with confirmed cases or possible infections with COVID-19. Due to being in close contact with patients, their job gives them an increased risk of exposure to this virus.
How to protect yourself while caring for patients:
There are steps health care workers can take to minimize their chance of being exposed to COVID-19 when caring for confirmed or possible patients. The CDC has infection prevention and control guidelines for health care workers, including use of recommended personal protective equipment.
The CDC defines personal protective equipment (PPE) as a main source of protection for emergency and recovery workers which is necessary to provide protection from physical, chemical and biological hazards.
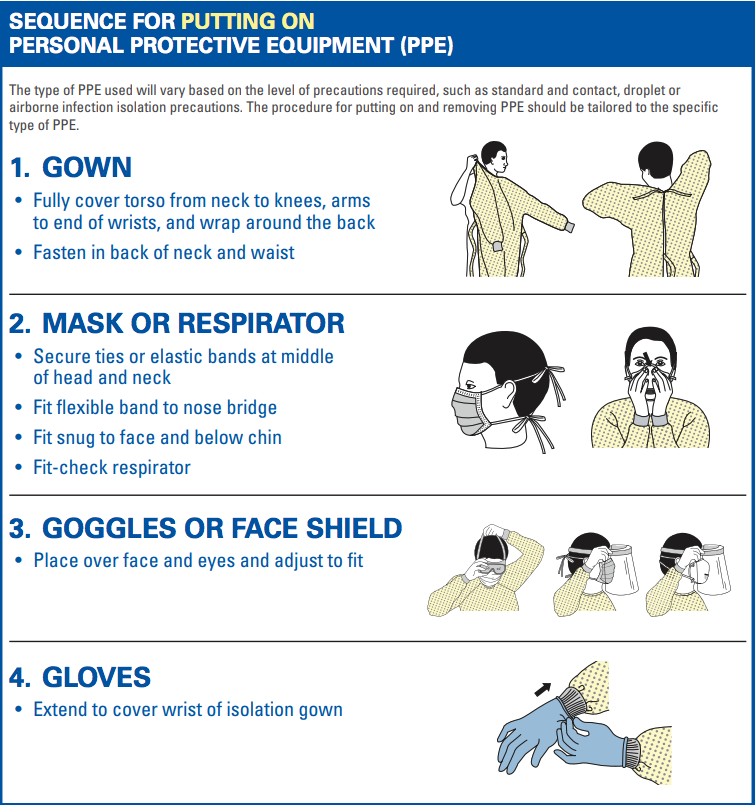
Recommended PPE:
- A single pair of disposable patient examination gloves. (Change gloves if they become torn or heavily contaminated)
- Disposable isolation gown
- Respiratory protection
- Eye protection (goggles or disposable face shield that fully covers the front and sides of the face)
The CDC has specific protocol for how to put on PPE:
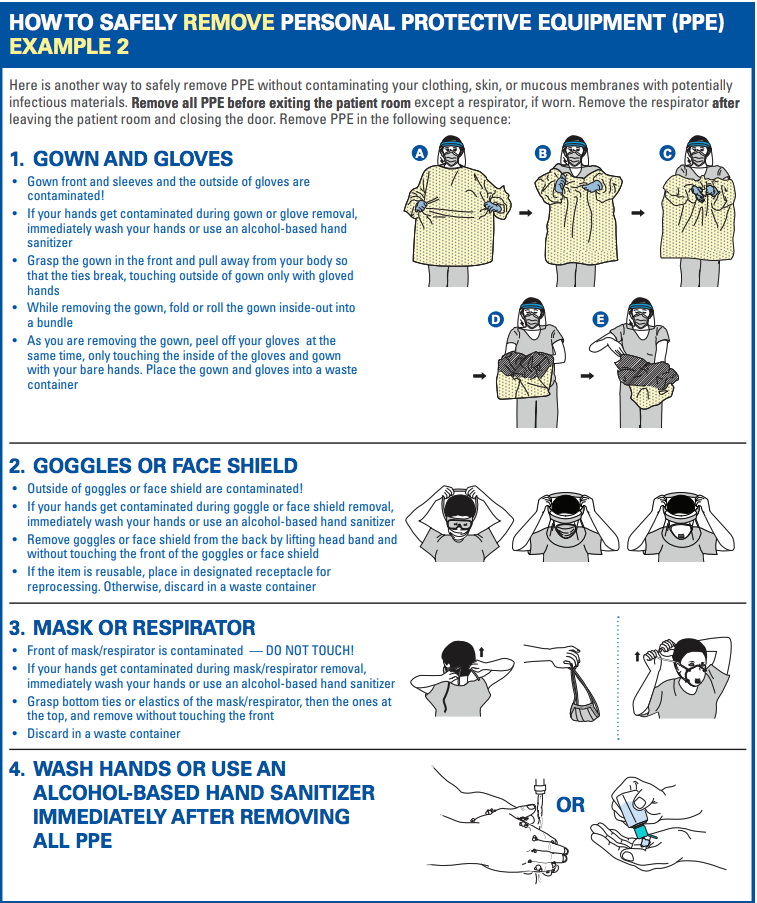
When it comes time to remove PPE, the CDC reminds health care workers that the front of the gown, sleeves, and outside of the gloves are considered to be contaminated. Extra precaution should be taken to ensure none of your bare skin touches the contaminated material.
All PPE should be removed before exiting the patient’s room, except if you are wearing a respirator.
To remove the gown:
- Grasp the gown in the front and pull away from your body so that the ties break. Make sure to only touch the outside of the gown with your gloved hands.
- When removing the gown, roll or fold the garment inside-out and into a bundle.
- As you are removing the gown, peel off your gloves at the same time, only touching the inside of the gloves and inside of your gown with your bare hands.
- Place the gown and gloves into a waste container.
After all of the PPE has been removed, it is important to wash your hands for a minimum of 20 seconds or use an alcohol-based hand sanitizer.
Tips For First Responders:
- EMS workers should notify the receiving health care facility that the patient has an exposure history and signs and symptoms suggestive of COVID-19
- Keep the patient separated from other people
- Family members and other contacts should not ride in the transport vehicle
- Isolate the ambulance driver from the patient compartment
- Keep pass-through doors and windows tightly shut
- When possible, use vehicles that have isolated driver and patient compartments that can provide separate ventilation to each area.
- Close the door/window between these compartments before bringing the patient on board.
- During transport, vehicle ventilation in both compartments should be on non-recirculated mode to maximize air changes that reduce potentially infectious particles in the vehicle.
- If the vehicle has a rear exhaust fan, use it to draw air away from the cab, toward the patient-care area, and out the back end of the vehicle.
Mask-Wearing Tips for the General Public:
People are increasingly adopting the use of cloth face masks to slow the spread of COVID-19, and the latest science may convince even more to do so. In an article published in the Journal of the American Medical Association this past July, the CDC reviewed the latest science and affirms that cloth face coverings are a critical tool in the fight against COVID-19 that could reduce the spread of the disease, particularly when used universally within communities.
There is increasing evidence that cloth face coverings help prevent people who have COVID-19 from spreading the virus to others.


CDC Guidelines for the Holidays:
While the holidays are traditionally meant for spending time with family, friends, and loved ones, the CDC is recommending people take extra precautions this year. This is for both the safety of the public and the health care workers, as hospitals are becoming overwhelmed with patients.
The CDC states that celebrating virtually or with members of your own household poses the lowest risk for spread. People who do not currently live in with you, such as college students who are returning home from school for the holidays, should be considered part of different households despite the fact that they may be family. In-person gatherings that bring together family members or friends from different households, including college students returning home, pose varying levels of risk, according to the agency.
Organizers and attendees of larger events should consider the risk of virus spread based on event size and take steps to reduce the possibility of infection, as outlined in the Considerations for Events and Gatherings.
There are several factors that contribute to the risk of getting and spreading COVID-19 at small in-person gatherings. In combination, these factors will create various amounts of risk:
- Community levels of COVID-19 – High or increasing levels of COVID-19 cases in the gathering location, as well as in the areas where attendees are coming from, increase the risk of infection and spread among attendees. Family and friends should consider the number of COVID-19 cases in their community and in the community where they plan to celebrate when deciding whether to host or attend a gathering. Information on the number of cases in an area can often be found on the local health department website.
- Exposure during travel – Airports, bus stations, train stations, public transport, gas stations, and rest stops are all places travelers can be exposed to the virus in the air and on surfaces.
- Location of the gathering – Indoor gatherings, especially those with poor ventilation (for example, small enclosed spaces with no outside air), pose more risk than outdoor gatherings.
- Duration of the gathering – Gatherings that last longer pose more risk than shorter gatherings. Being within 6 feet of someone who has COVID-19 for a cumulative total of 15 minutes or more greatly increases the risk of becoming sick and requires a 14-day quarantine.
- Number and crowding of people at the gathering – Gatherings with more people pose more risk than gatherings with fewer people. CDC does not have a limit or recommend a specific number of attendees for gatherings. The size of a holiday gathering should be determined based on the ability of attendees from different households to stay 6 feet (2 arm lengths) apart, wear masks, wash hands, and follow state, local, territorial, or tribal health and safety laws, rules, and regulations.
- Behaviors of attendees prior to the gathering – Individuals who did not consistently adhere to social distancing (staying at least 6 feet apart), mask wearing, handwashing, and other prevention behaviors pose more risk than those who consistently practiced these safety measures.
- Behaviors of attendees during the gathering – Gatherings with more safety measures in place, such as mask wearing, social distancing, and handwashing, pose less risk than gatherings where fewer or no preventive measures are being implemented. Use of alcohol or drugs may alter judgment and make it more difficult to practice COVID-19 safety measures.
No matter how you spend the holiday season, all of us at Intiva Health hope that you have a safe, happy, and healthy holiday, for the sake of yourselves, your loved ones, and all of the health care workers on the front lines.
Related Posts: