Provider credentialing vs. provider enrollment:
This white paper is an overview of the required credentialing process that a medical provider must complete and how it is distinct from the enrollment procedure that facilitates eligibility to accept patients and receive payments through a commercial insurance provider or government health plan.
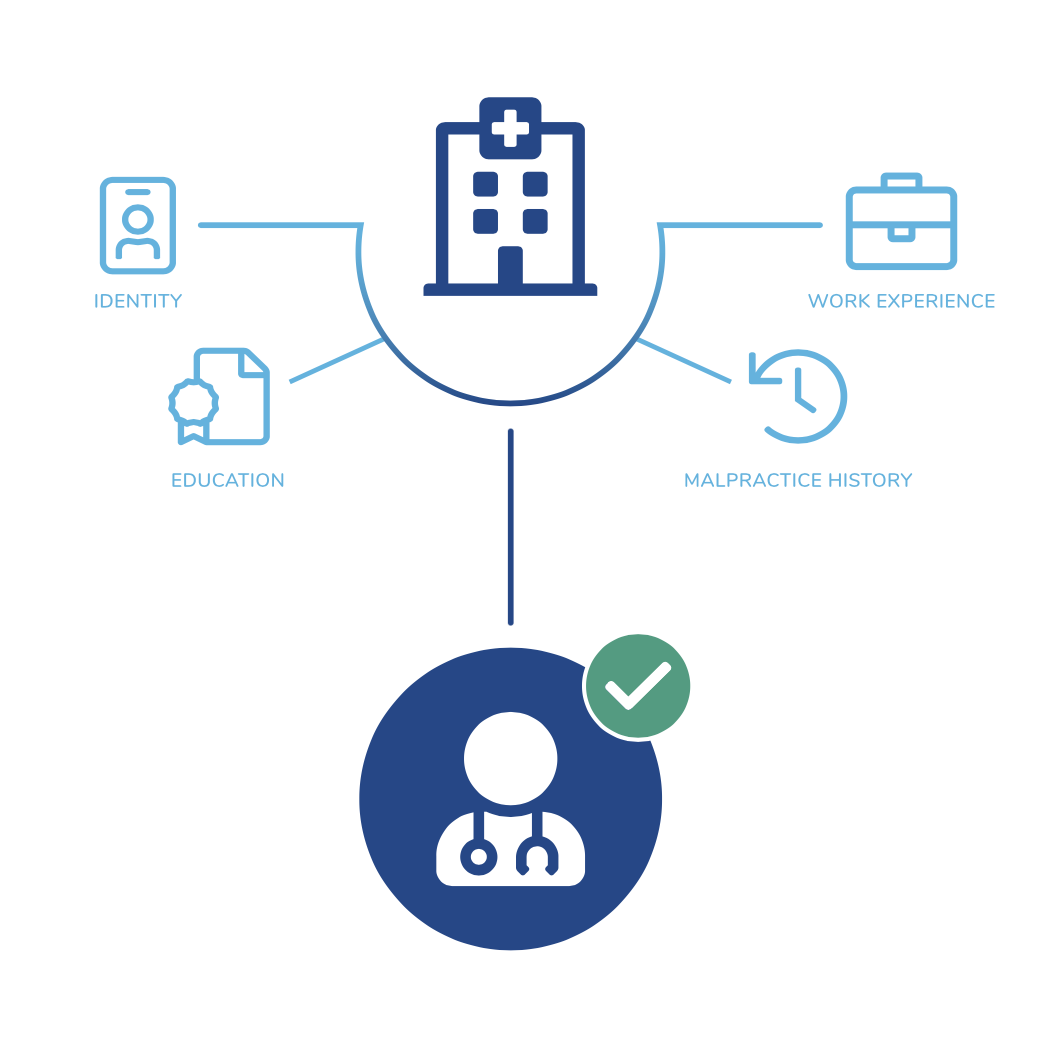
The Credentialing Process
This white paper is an overview of the required credentialing process that a medical provider must complete and how it is distinct from the enrollment procedure that facilitates eligibility to accept patients and receive payments through a commercial insurance provider or government health plan. Provider credentialing and provider enrollment are two essential processes that must be completed in order for a health care provider to begin working in the industry and receive reimbursement payments from a health insurance plan.
Provider Enrollment
Enrollment refers to the process of a health care provider requesting participation in a health insurance plan network. It can also be the validation of a provider in a public health plan such as Medicare or Medicaid and the approval to bill the agency for services rendered.
It is important to note that enrollment is entirely independent from credentialing, yet the latter is a prerequisite for the enrollment process to occur. Therefore, credential management directly affects a provider’s enrollment options and outcomes.

Download the full whitepaper
Like what you read so far? Fill out the form below for your very own copy!