The Pulse
3 Ways Faster Credentialing Can Improve Healthcare in America
Category: Credentialing
It can take anywhere from a few weeks to six months to get credentialed.
For physicians, that’s over three hours spent submitting around 20 different credentialing forms, according to the New England Journal of Medicine (NEJM). Then facility staff spends an additional 20 hours on each physician’s forms. If anything is missing from the application or a school, employer, or reference doesn’t swiftly respond to verification requests, it can add weeks or even months to the process.
This has to be re-done every two years, on top of continuing medical education (CME) requirements. That, combined with other non-clinical paperwork, takes up 8.7 hours a week for the average doctor, according to a National Center for Biotechnology Information (NCBI) study.
Each facility has its own way of managing credentials, too, collecting the same information as everyone else and often ignoring national databases that could make the process simpler. It’s a “mess that just gets worse and worse” and “takes many hours and causes many headaches,” wrote physician and author Christopher Johnson, MD on KevinMD.
But what if provider credentialing could be done much quicker and easier? Here are three ways that would improve healthcare in America.
1. Doctors could start work sooner
Imagine if healthcare professionals could start their jobs weeks or even months sooner.
That would mean earning the income they would have earned if they weren’t waiting around to be credentialed. For a physician making the average annual income of $299,000, waiting a few weeks to be credentialed would cost them around $25,000 in lost income. Waiting six months, as some have had to do, would cost them around $150,000 in lost income.
A lot of physicians fall somewhere in between those two extremes, losing as much income waiting to get credentialed as many Americans make in a year.
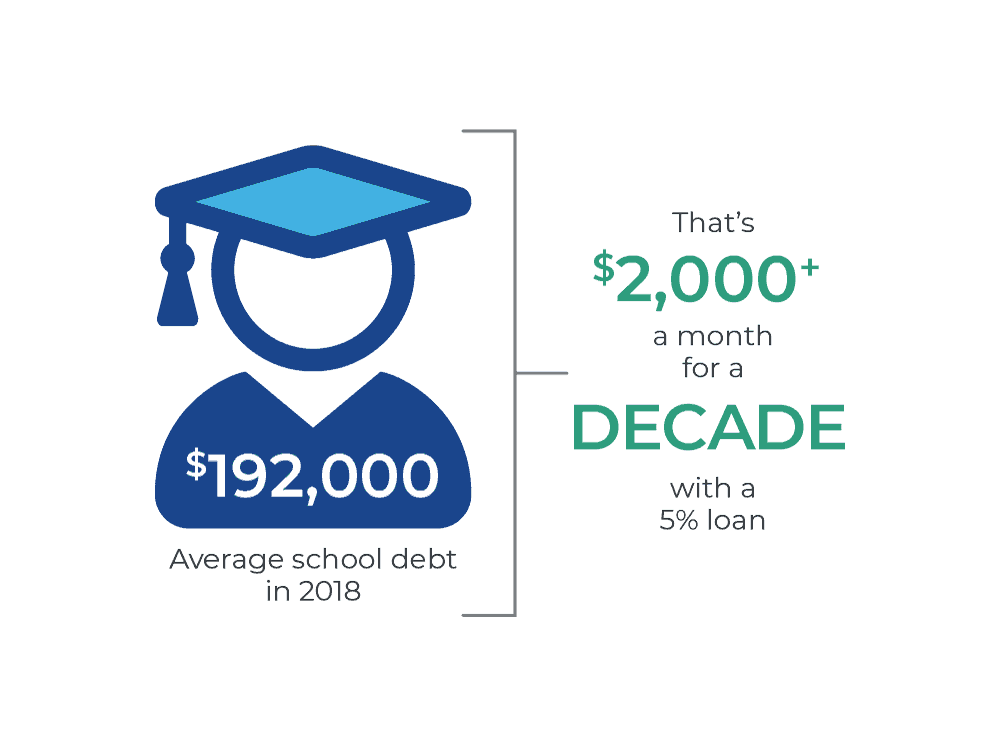
There’s a lot that can be done with that extra money, but it’s especially helpful for recent medical school graduates, whose average school debt was $192,000 in 2018, according to the Association of American Medical Schools. On a 10-year repayment plan for a 5 percent Perkins Loan, that comes out to a bill of just over $2,000 a month. On a 7.6 percent Direct PLUS Loan, they’d have to pay nearly $2,300 a month.
With a monthly bill that high, they really can’t afford to be in-between paychecks. They need money to survive and to start knocking down that enormous debt, which can be done much quicker if they can start their jobs sooner.
Physicians being able to start work sooner also means they get to see patients sooner, which is the reason most doctors enter the field in the first place, according to St. George’s University research. Who wants to let their education go to waste when people need help? It’s lose-lose.
2. The industry could save billions
Credentialing inefficiencies in America don’t only affect doctors: They affect the entire industry.
According to a widely cited Institute of Medicine study, the United States spends an estimated $361 billion a year on healthcare administration, with half of that being unnecessary. While not all of that is spent on credentialing software, credentialing still costs individual hospitals millions of dollars a year, according to NEJM.
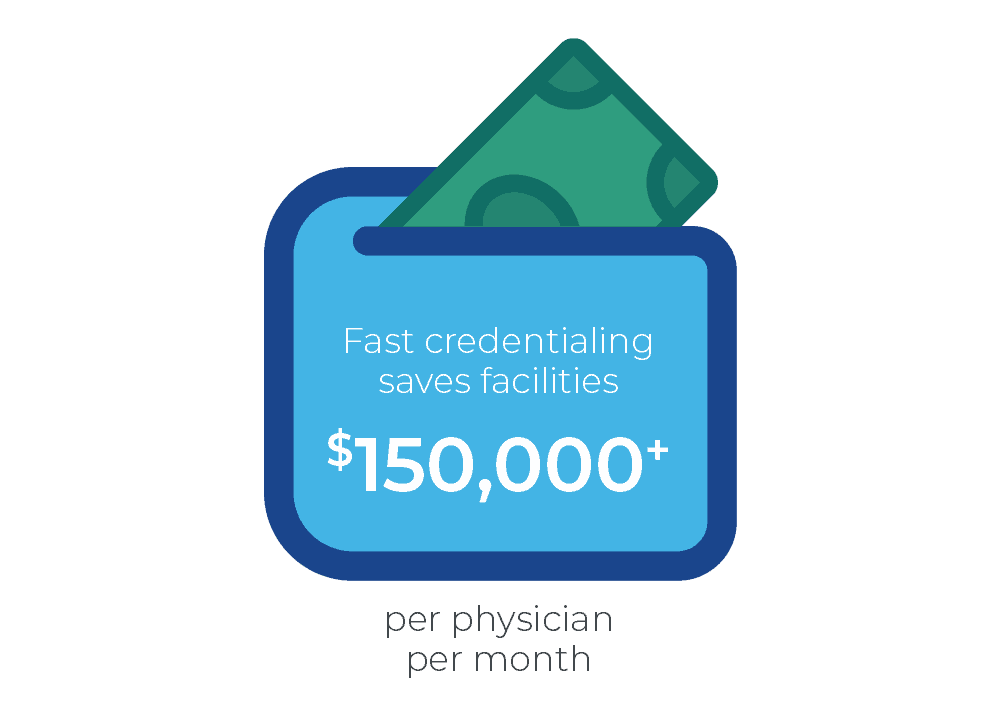
A lot of that lost revenue comes from the credentialing process postponing physician start dates. As a Merritt Hawkins survey found, a physician earns a facility an average of $2,378,727 per year. If credentialing that physician takes six months (worst-case scenario), that’s $1,189,363 of lost revenue for that facility. Even if credentialing only takes a few weeks (best-case scenario), the facility still loses around $150,000.
Imagine if that process could be done much quicker. Not only would that save hours of work for each facility, it’d also save an incredible amount of money, which could be reallocated toward better patient care. An improvement in quality care could further boost revenue if happy patients post positive reviews online, potentially increasing a facility’s ranking on the U.S. News & World Report.
Facility savings would also lead to improved physician satisfaction, according to NEJM, since it’d allow them to have more time and resources for direct patient care. And that lack of feeling rushed would likely reduce burnout—something that affects 54.4 percent of all physicians and 63 percent of family physicians, according to a study by the Mayo Foundation for Medical Education and Research.
This problem literally hurts everyone.
3. Patients could receive better, more efficient care
Doctors starting work sooner and facilities saving millions both lead to better patient care.
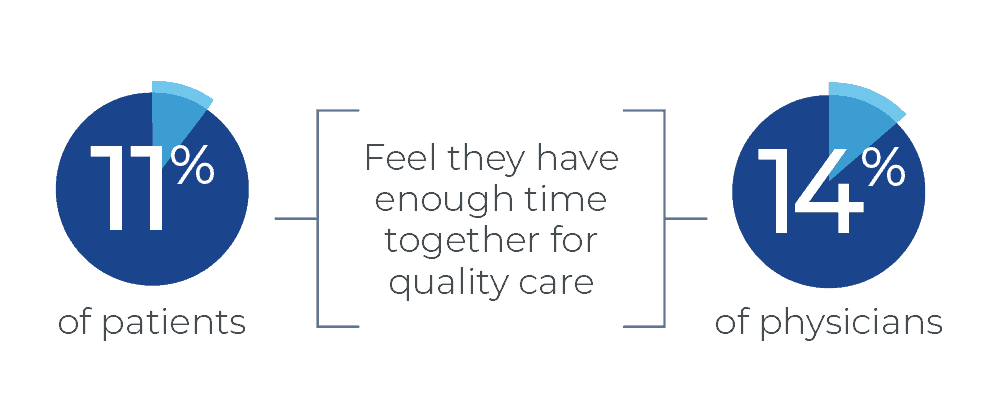
A physician starting work sooner puts one more doctor on the floor. More working doctors leads to less time in waiting rooms and more time being seen. That’s something that’s important to both physicians and patients alike, according to a survey by The Physician Foundation, which found that only 11 percent of patients and 14 percent of physicians feel enough time was allotted for the highest standards of care.
That alone could be life-saving, according to Robb Duke, VP of Intiva Health.
“If doctors spend 8.7 hours a week on non-clinical paperwork, that’s time they’re not seeing patients, or worse, not sleeping,” Duke said. “If you can give a doctor those hours back, they can spend more time getting a better perspective before making a decision about care. Even having more time to sleep the night before seeing a patient could lead to a better diagnosis.”
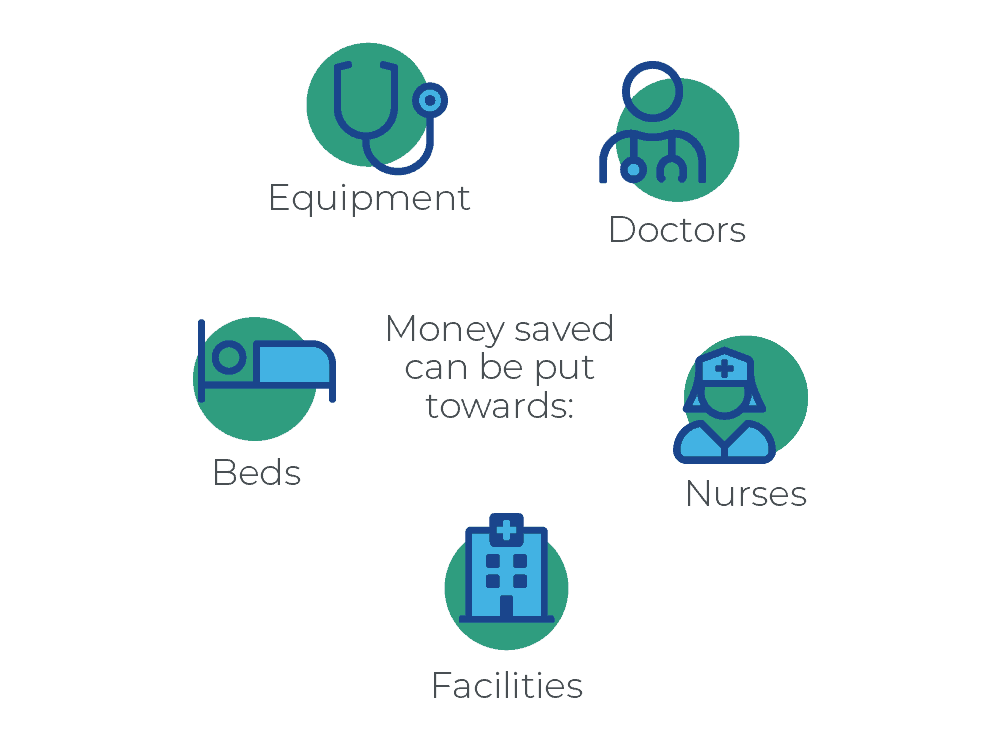
Plus, by facilities saving millions a year on credential management, more money could be put toward buying better equipment, hiring more doctors and nurses, getting more beds, opening up more facilities, and so on. It all comes back to the patient, which at one point or another, is everyone.
Faster credentialing is here
There’s already a way to drastically speed up credentialing, and that’s through Intiva Health, which uses Hashgraph technology to cut down credentialing from months to minutes.
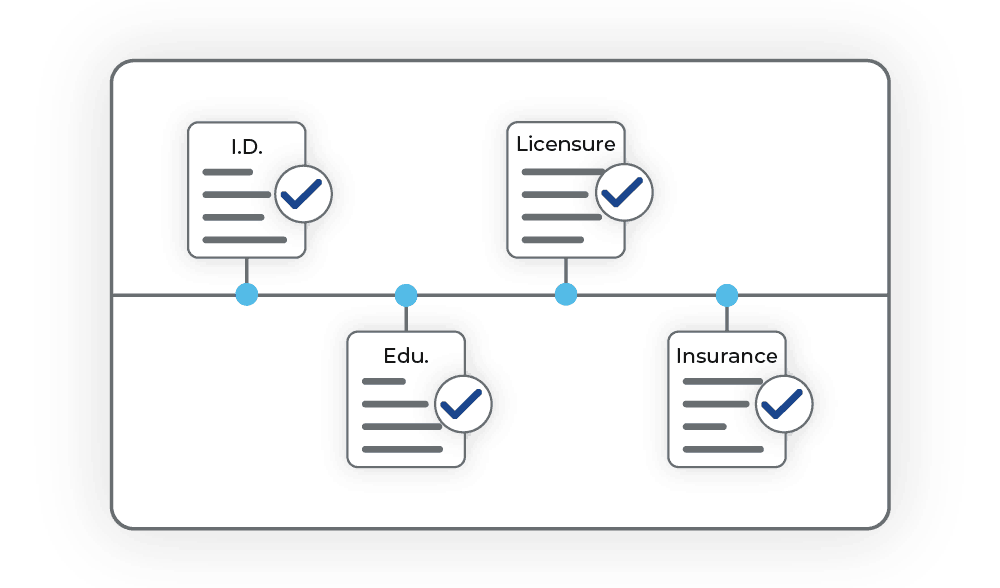
The way it works is healthcare professionals upload their credentials to the Intiva Health platform, allowing facility staff, practice managers, CVOs, etc. to review and share these documents. Once verified, Hashgraph then creates a date and timestamp, using a consensus algorithm, to ensure these documents don’t get tampered with. This allows credentials to only have to be reviewed once, so no one has to spend additional weeks or months verifying something that’s already been verified.
After the initial credentialing process, physicians are required to maintain licenses and stay credentialed by taking free CME courses and keeping track of their CME certificates, which is also something Intiva Health offers. Having all of the courses you need in one place (often for free) expedites this ongoing process even further.
Overall, faster medical credential management eliminates all of the inefficiencies that postpone physician start dates, cost the industry billions of dollars, and reduce the quality of patient care.
“There are real-world implications to these inefficiencies,” Duke said. “This is a billions-a-year issue that points to a bigger systemic problem that Intiva Health can help fix.”