The Pulse
Health Care Industry Losing Time, Money With Current Credentialing Methods
Category: Credentialing
IN A NUTSHELL:
- Current credentialing methods take 55 days on average
- Facilities lose $400,000 in revenue on average per physician
- Widespread lack of awareness exists concerning credentialing software
A recent survey (.pdf) focusing on the common methods utilized by the health care industry for credential management revealed various inefficiencies. The survey, conducted by Intiva Health, involved workers within the health care sector across all regions of the U.S.
Participants detailed the time-intensive process involved in health care credentialing, the low-level of confidence when utilizing in-house credentialing software, and the burden of responsibility that is often placed upon a single individual which detracts from the ability to perform their primary job responsibilities.
Results illustrated that the credentialing process for a single provider takes nearly two months on average to complete.
The consequence is hospitals and other health care organizations often view credentialing as a regulatory burden. Despite the importance of maintaining up-to-date credentials for patient, provider, and institutional protection, most health care organizations only check credentials at the time of hire and then once every two or three years.
In combination with other non-clinical paperwork, the administrative burden of the credentialing process takes up nearly nine hours a week for the average doctor. Then, facility staff spends an additional 20 hours per form.
If any elements are missing from the application, or if a school, employer, or reference doesn’t swiftly respond to verification requests, it can add weeks or even months to the process.
All of this time spent waiting on the credentialing process to be completed is precious time lost that could be utilized focusing on patient care, and ultimately represents a loss of revenue for the health care facility.

Additionally, the survey showed that a lack of awareness exists concerning the availability of software that can offer an electronic, streamlined approach to credential management. Time, money, and resources are all sacrificed to complete a process that is legally required and necessary for quality health care services and successful business operations.
Despite all of the intricacies involved with credentialing, a majority of health care workers still endure the process either manually, with electronic spreadsheet documents, or proprietary software.
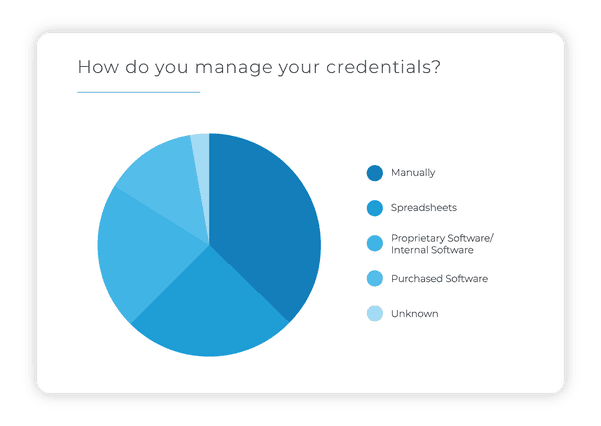
However, our survey shows that none of these methods provides complete confidence that they are executing the process correctly or efficiently.
IN DEPTH | View the full survey analysis
The administrative burden associated with the manual process, and a failure to implement automated systems that would ease the burden and ensure consistent compliance, directly results from a lack of awareness and lack of understanding concerning the cost benefits, risk mitigation, and general efficiency of an electronic credentialing system.
Related Posts: