![]() CREDENTIALING
CREDENTIALING
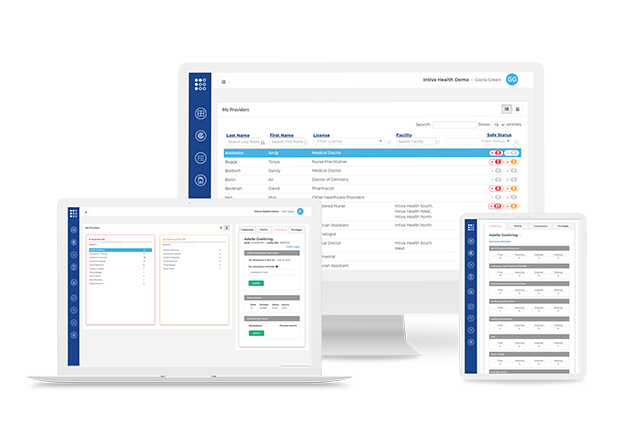
MEDICAL CREDENTIALING SOFTWARE
The solution is a win-win for providers, patients, and facilities! The credentialing process is fast and hassle-free. With our credentialing software providers can start treating patients sooner, revenue is boosted, administrative work is reduced, and there is more time for patient care.
Save Money
Medical credentialing can take anywhere from a few weeks to six months, while facilities lose on-average $1.2 million in revenue per physician. Healthcare Providers themselves lose tens of thousands of dollars in revenue waiting on credentialing. Let us help you get that money back.
Save Time
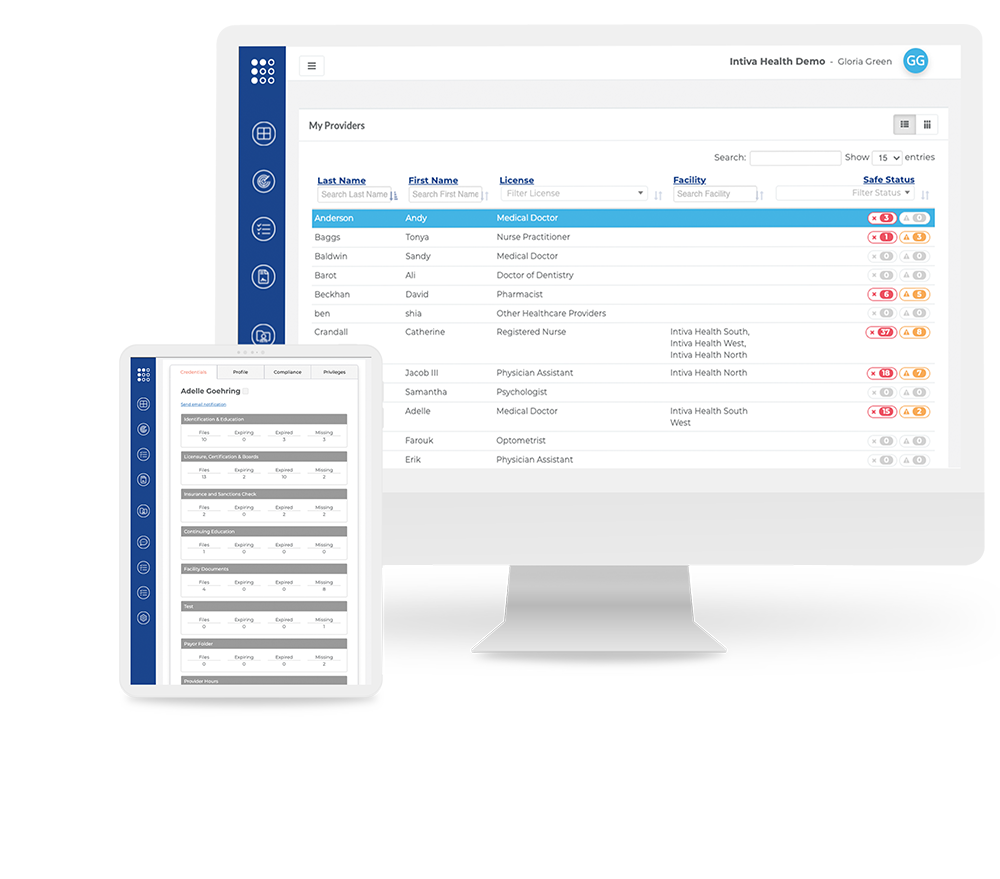
Providers or facilities can upload credential documents to the Ready Doc™ platform, allowing facility staff, managers, and CVOs to review and share the documents. This means spending less time on credentialing, privileging, and payor enrollment–leading to more time for patient care.
Reduce Risk
Databank monitoring and automated alerts for expiring medical credentials helps providers and facilities alike reduce the risk of a compliance breach.
- PROVIDER

- FREE, FOREVER







- CREATE ACCOUNT
- FEATURES
- DLT SECURITY


Using distributed ledger technology (DLT), all documents uploaded to Ready Doc are assigned an unalterable and secure timestamp using a consensus algorithm that ensures reliability. - CREDENTIAL STORAGE


Upload, share and track documents of any kind. A healthcare-specific folder structure provides a convenient method of organization for standard. - EXPIRATION ALERTS


Receive alerts about credentialing documents or malpractice insurance far in advance to avoid penalties and ensure compliance. - APPOINTMENT TRACKING


In addition to tracking credentials, administrators can also track provider appointments directly f rom the dashboard. - PRIVELEGES TRACKING


Administrators can easily track a provider’s delineation of privileges f rom the Ready Doc dashboard. - TASK MANAGER


Create and track tasks of any kind that involve your administration, providers, facility, and more, all in the same platform. - BASIC MONITORING


Quickly identify OIG excluded individuals and mitigate federal reimbursement ineligibility risks. - BASIC REPORTS


Leverage existing reports or generate custom reports and export the documents in a file type that is easy to share. - PROVIDER ROSTERS


Manage all of your providers in a centralized database. Whether you want to notify them of expiring credentials or tell them to upload documents to the platform, it can be done with a single click. - MANAGE PAYERS


The manage payers feature streamlines the payer application process and takes the tracking of provider information to another level. Hundreds of payers are already uploaded into the system, allowing users to connect providers with specific payers to begin the enrollment process. - CUSTOM DOCUMENT DESIGN

Branded, accurately formatted versions of your documents are available with a click, from any device, location, and access them anytime, anywhere. They’ll look great—and work great—every time. - AUTOMATED DATA ENTRY


No more manual data entry of provider data in application documents. Your documents will always be accurate, pulling data from your provider roster and placing them in the correct place for meaningful communications withno errors. - E-SIGNATURE


Simplify the process of working with providers by offering them an easy, secure way to sign documents. Track every document from draft to completion in real-time, while sending and receiving documents within minutes - CONTINOUS MONITORING


Monthly monitoring of Medicare and Medicaid sanctions as well as state licenses and DEA are available with Ready Doc Credentialing PLUS. Notifications are sent immediately when disciplinary actions are discovered. - PRIMARY SOURCE VERIFICATION


Dedicated credentialing support specialists assist healthcare organizations and providers throughout the process. Our support team provides status reports on all credentialing projects including 30/60/90 day prior notifications of expired licenses, hospital or facility re-credentialing needs or malpractice expiration.
- FACILITY

CREDENTIALING- FREE, FOREVER









- –
- –
- –
- –
- –
- –
- SCHEDULE DEMO
- FACILITY
CREDENTIALING PLUS














- SCHEDULE DEMO
- REQUEST PRICING
Latest reviews for Ready DocTM
The feature that I like most about Ready Doc is the simplicity of the platform. It is very user-friendly and if there are any issues, customer support is there to help.
- Sheli C.
User friendly interface, great customer service & tech support. It's great to see all vital information at a glance.
- Lynn H.
The software is very simple to use and easy to navigate.
- Rachel Q.
100+
Ready DocTM facilities
60265
Ready DocTM medical providers
Frequently asked questions
Who can use Ready Doc™ Credentialing?
If you manage any type of licensed medical professional – Ready Doc™ Credentialing is your solution to better provider management. We’ve automated and streamlined the credentialing management process for many types of facilities, such as Hospitals, ASCs, FQHCs, MCOs, staffing companies, and medical clinics. Schedule a product tour today to see how Ready Doc™ Credentialing can save your resources!
What is medical credentialing?
Medical credentialing is the process in which medical facilities and groups review licensed health professionals’ qualifications to ensure they have the required experience and training to safely and effectively practice medicine. These qualifications include medical licenses, specialty certificates, education training, work history, residency, and other training. This credentialing process must be completed each and every time a health care worker starts at a new practice. Following the initial credentialing process, a health care worker must be re-credentialed every two years.
How long does it take to get credentialed?
The amount of time it takes to get credentialed can greatly vary. If a provider submits all of the necessary paperwork in a timely manner, all of the information is accurate and complete, and all verification requests are successful, then the credentialing process can be done within weeks. If any of these steps are delayed, credentialing medical staff can take up to six months. With Ready Doc™, the entire credentialing process is expedited. Ready Doc™ uses Hashgraph technology allowing documents to only have to be verified one time—eliminating a redundancy that costs months of lost income.
Does Intiva Health offer credentialing?
No. We’re not a CVO (Credential Verification Organization). Much like the National Committee for Quality Assurance (NCQA), and The Joint Commission (TJC) we’re a useful tool you can use during the credentialing process. The difference is that Ready Doc doesn’t actually offer credentialing services. Instead, we’re a credential management platform that lets you manage, organize, and share your credentials in a swift, secure way.
How is credential management different from credentialing?
Credential management software, which is what Intiva Health offers, helps make the medical credentialing process easier. We give you a central place to upload, manage, organize, and share credential documents to speed up verification from months to minutes. Credentialing is merely the process we’re helping you with, but we don’t actually do it for you like a CVO would. This is actually better, though, because it allows you to have control over the credentialing solution while letting us keep our services completely free.
How much does Ready Doc cost?
The basic version of Ready Doc™ is free for both administrators and their medical staff. It will always be free, too, which sets us apart from other medical credentialing software. We also offer enhanced, premium features for a small, additional fee.
Does Intiva Health offer provider enrollment for insurance plans?
One of the premium features of Ready Doc™ allows administrators to automate provider enrollment by populating information into a digital form. Ready Doc™ contains a variety of application templates ready for use in the system, and the enrollment process can also be completed with our eSignature feature.
How can Ready Doc™ help with compliance?
The work does not stop after a provider has completed the credentialing and enrollment process. Ready Doc™ also offers several compliance features including automated alerts for expiring documents, monitoring for OIG exclusion and sanctions, and HIPAA-compliant messaging solutions. Intiva Health also offers the ability to purchase cyber breach insurance plans through a partnership with Lloyd’s of London.
Schedule a Free Demo
Fill out the request form below to get a
free demo of the Ready DocTM platform.







